The following piece discusses su*c*e. If you have experienced s****dal thoughts or have lost someone to s****de and want to seek help, you can contact Suicide Prevention Lifeline (Kaan Pete ROI) |GP: 01779554391, 01779554392 |Airtel: 01688709965, 01688709966| Banglalink: 01985275286 |Robi: 01852035634|
A study published in March 2021 found that 14,436 people in Bangladesh had taken their own lives since March 2020- 70% more than coronavirus claimed during that period.
Why is the number so high one might wonder? Probable causes include but are not limited to social isolation, depression, anxiety, physical or emotional abuse, financial instability, and the list goes on.
While we might criticize death is not a practical solution, it is to be established that for the people who attempt or commit suicide, they were not choosing it as the most efficient solution to begin with. They ‘feel’ as if they had run out of all solutions that they could think of and lose all hope of the situation getting better, and hence, they want ‘out’. The combined psychological impact of the problems they face are complex, the series of issues are often rather deeply rooted, and we should not expect any and all solutions available for suicidal people should heal them overnight.
One solution does not fit all.
But everyone deserves the opportunity to get help at their lowest point. Unfortunately, treatment for mental illnesses/disorders is extremely inaccessible in Bangladesh. Today, we will be discussing the reasons behind this scenario.
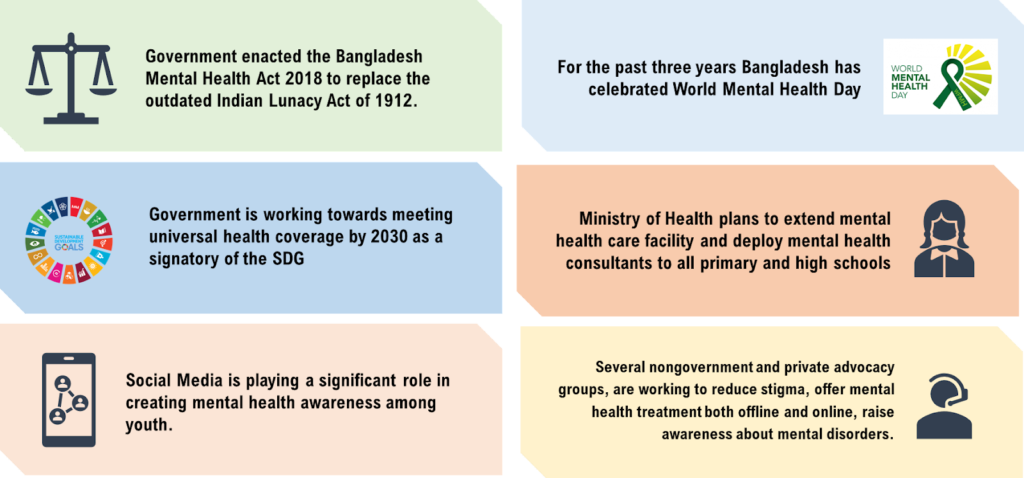
In recent years, there have been several initiatives taken up by the government and private organizations to improve the situation:
Despite all these initiatives, people find it difficult to seek help for their mental health struggles for the following reasons:
The Social Stigma of Being a “Lunatic”
Just like hundreds of other things of our conservative society, mental health, too,is a taboo topic. We don’t discuss our mental health issues because we don’t want to be perceived as weak, incompetent, or unstable.
Our judgmental society jumps up at the chance of labeling those who show any signs of mental disorders as “attention seeking” or “lazy”. This judgment is more deeply rooted in families where parents did not take care of their own mental health. Their main argument is often,
“We have faced so many challenges in our lives, why are you so weak? You are the one who’s always complaining. Look at the things you already have and be grateful for them.”
Saying these to kids is not only unhelpful but saying these to a child with depression could also push them further away from their family and increase their loneliness and frustration. Invalidating mental health issues for an extended period of time poses long-term effects. Often the cycle of generational trauma continues because as the parents are not aware of their mental health, they cannot control how their dysregulation of emotions impacts their children’s lives as well.
We have a cultural distrust of mental health struggles because we cannot distinguish them easily like physical diseases.
According to the National Mental Health Institute of Bangladesh, nearly 17% of adults in Bangladesh are suffering from mental health issues, and among them 92.3% do not seek medical attention.
In rural and suburban areas, every mental issue is treated as “possession by spirits” or “insanity”. Most of the time, they abuse the person with mental health issues or exclude them from their communities. Sometimes, they are hidden away by their families and forced to live in isolation.
Even after all this stigma, some people do try to seek medical help. But generally, they are left disappointed by the lack of accessibility, poor condition of our mental health facilities and not-so-qualified mental health experts.

Abysmal Condition of Mental Health Facilities
There is a huge discrepancy between planning and execution when it comes to mental health care activities in Bangladesh. While there are steps being taken for the betterment, it is not enough.
- The public spending on mental health is approximately 0.08 USD per capita, representing 0.05% of the total health budget.
- There is only 1 mental health specialist for every 800,000 people.
- There is no specific mental health authority in the country.
- Adequate psychiatry learning is not included in the undergraduate medical curriculum (MBBS).
- Only 20 students are enrolled per year in each post graduate course, which does not allow to meet the country’s need for psychiatrists.
- There is no facility for follow-up care in the community
The only government run mental hospital in Bangladesh is Pabna mental hospital which has only 500 beds. The pictures below were taken inside Pabna Mental Hospital by photojournalist Allison Joyce and published in The Guardian.

When there is such limited infrastructure, clinics, or services to access for support, it is impossible to deliver quality mental health treatment. The harm, the lack of the above results in, is that often in addition to being stigmatized and socially shunned, the mentally vulnerable patients also receive mistreatment and negligence from their assigned healthcare professionals. This can result in their mental health declining even faster, and hence more harm than good might be caused in the attempt. Thus the possibilities further demotivate people to seek mental health treatment institutionally.

Mental health awareness is a comparatively new addition to urbanization. Most of the mental health care facilities are city-based. Unfortunately, 74% of Bangladesh’s population is rural. So, statistically, there are more people with undiagnosed mental health issues in the rural areas than in the urban areas.
Rural people are dependent on traditional faith healers (religious leaders, pirs or shamans) for treating mental health because they believe they have no other choice. And unfortunately, it is true.
In addition to the lack of awareness regarding mental health and mental health care facilities, there are no qualified experts in the rural area. These roadblocks lead the rural people to fall into the traps of faith healers who abuse the patients and call it “treatment”.
In the city, unfortunately, the situation is no better. Only the upper class can afford quality mental health care. The scarcity of good mental health professionals has made them less affordable for the middle and lower-income people. For this reason, many treat mental health as a “rich person’s problem” in our country.
Unpleasant Experiences with Specialists: When Your Doctor is Your Worst Nightmare
Even when people can afford mental health care, many people do not want to repeat the process due to lack of proper care in mental health facilities and absence of professionalism in many mental health experts.
It is true that finding a therapist who can cater to your needs properly is a complicated process. But it is 100 times harder to find one in Bangladesh simply because the pool to pick from has next to none.
The key issues patients face is:
- Generational gap leads to older mental health professionals undermining issues faced by adolescents and young adults.
- Patient’s confidentiality is challenged due to lack of professionalism.
- Misdiagnosis of disorders and suggesting medication as the only resort.
All these issues can be solved if the professionals were well trained and not just degree holders. Yes, being bad at your job is not uncommon, but it becomes extremely detrimental when your job is to protect people’s lives- people who are at the verge of ending it themselves. It is unfortunate that mental health professionals in Bangladesh don’t seem to hold themselves accountable for their actions.

The Road Ahead…
For making mental health treatment easily accessible to the public, several steps should be taken by the government. These includes:
- Boosting the budget allocation for mental health by Government
- Proper integration of mental health into primary health care
- Introduction of an official mental health authority under ministry of health
- Proper implementation of a National Mental Health Strategic Plan 2020-2030
- Upgradation of MBBS curriculum with inclusion of psychiatry in an optimum stake,
- Development of psychiatric unit at district level, and in all medical colleges
But we all know that execution of these steps will take decades because of bureaucracy, corruption and most importantly, people’s ignorance. That’s why spreading awareness and correct information about mental health is the most significant step that can help people. Extensive awareness programs involving electronic and printing media and the inclusion of mental health-related topics in school curriculum will directly help people be more aware about mental health. The rural people are the most vulnerable when it comes to mental health awareness, so more focus should be on developing rural based awareness programs.
Non-government organizations like the Shuchona Foundation, LifeSpring, Sajida Foundation, Moner Bondhu, Moner Daktar, Innovation for Wellbeing, and Walk to Serenity have been offering easy access to mental health experts and raising mental health awareness. We need more initiatives like these organizations to promote mental health literacy.
At the end of the day, we should be empathetic, kind and understanding towards people suffering from mental health issues. In our every day life it should be a constant reminder that not all struggles are visible; we do not know what the person next to us is going through. And if you know anyone is in pain, do not trivialize their trauma; listen to them, and tell them you are by their side no matter what.
Remember: One word of kindness can change someone’s bad day into a good one.